Trauma Training Tip
Touch the skin and touch the world for your patient!
Touch is our first sense. It is our first and most primal communication. Many people live without sight, hearing, smell or taste — but no one can survive without touch!
Our skin is a boundary organ. It is a relatively global tissue — bones and muscles have a beginning and an end — but our skin surrounds us. When we touch with attention on the skin, we touch our patient in a global way. We can inadvertently activate a memory of boundary violation if we are unaware of the impact of our touch.
Conscious touch can also restore a global sense of safe, secure and flexible armor for engaging the world. Trauma that occurred pre-verbally cannot be renegotiated with words; it requires safe, mindful, appropriate touch for it to be re-negotiated.
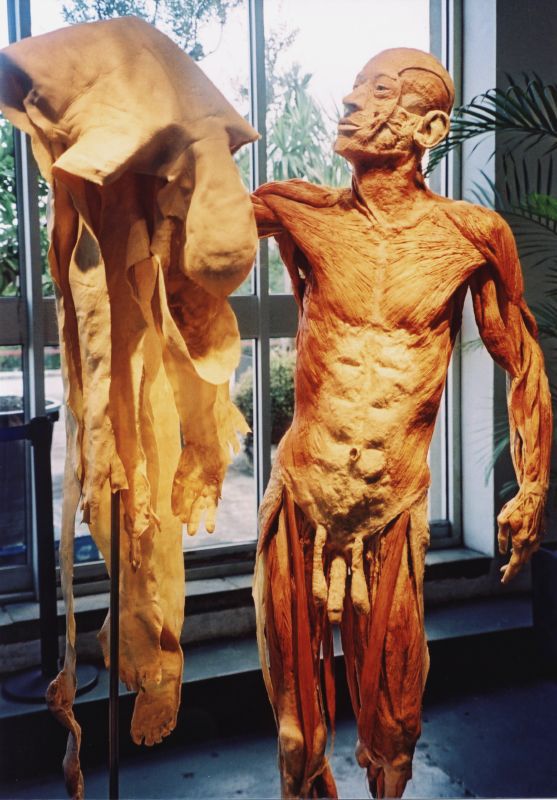 We access the Po/Animal Soul directly when we touch this essential container. The Po helps us make distinctions between self and non-self, and between excitation and threat. The skin has richly sensate experiences about the nature, location, quality and kind of touch it experiences and wants. It is an intelligent structure with lots of opinions and stored experiences!
We access the Po/Animal Soul directly when we touch this essential container. The Po helps us make distinctions between self and non-self, and between excitation and threat. The skin has richly sensate experiences about the nature, location, quality and kind of touch it experiences and wants. It is an intelligent structure with lots of opinions and stored experiences!
The skin is our largest organ and we penetrate it every time we needle a point. There are times we can’t and times we shouldn’t use needles. You may not have privileges in an in-patient setting, or there may be casting or local swelling that make needling ill-advised or impossible.
It also may not be clinically useful to use a needle when traumatic stress has resulted in either braced or collapsed tissue. Bracing constricts and obstructs movement of Qi; needling will be painful, and may result in even greater qi stagnation. Collapsed tissue lacks tone to carry Qi from a needle; you won’t get de qi, or a pulse change.
Touch can help with titrating the pace of your treatment. Distal attention with touch is less activating than local attention with a needle. Touch can help build the physiological capacity in your patient for needling to be tolerated and effective. Trauma survivors are complex; we need to explore multiple perspectives and find nuanced ways to restore regulation.
When we touch our clients, we are also being touched. Patients can experience safe co-regulation with another. They will feel safer and more regulated — and their Qi will be more available to your needle when you integrate mindful touch into your acupuncture treatments.
Check This Out!

The Science of Touching and Feeling | David Linden | TEDxUNC
David J. Linden, Ph.D., is a Professor of Neuroscience at the Johns Hopkins University School of Medicine. He is the author of Touch: The Science of Hand, Heart and Mind.
In this talk, David Linden explores the science and complexities of touch. Dr. Linden has some interesting observations: Touch is not optional for human development. Babies who are deprived of simple loving touch are more likely to develop obesity, diabetes, heart disease and mental illness. Basketball teams that celebrated successful plays with hugs, high fives and fist bumps early in the season display more cooperative, self-less behavior on the court and play more successfully. People who are gently touched by a server in a restaurant leave bigger tips. Doctors who touch their patients are rated as more caring and their patients have reduced stress-hormone levels and better medical outcomes.
Our gentle physical contact can help restore the neural deficits lost in pre and peri-natal trauma. We – and our patients — are fortunate that we are licensed to touch!
Alaine’s Two Cents
We are asking our patients to do a very complex thing: be immobilized and feel safe. If they did not have childhood experiences of being held in loving and playful ways, they may have difficulty discerning safety when they also feel over overpowered or immobilized. The dentist’s chair, a massage chair, some sexual postures can all trigger immobility/freeze responses. You standing over them with a sharp object may be activating – especially if they are undressed.
Pushing past their discomfort to “get the job done” will almost always turn into its opposite. Best not to needle into braced or collapsed tissue. Going slowly will build relationship, capacity and regulation faster for trauma survivors.
Clinical Curiosity
Where is your clinical curiosity carrying you?
Send me a question or two and I will explore them with readers in this corner next month.
Here’s one that recently came to me:
“My patient has so many things she is struggling with – but she won’t let me do very many needles. I know I could help her more if I could just convince her to let me treat more points.”
Many trauma survivors have complex, multi-symptom illness. Many also have hyper-sensitive responses to needles. It is a bit counter-intuitive, but I suggest that the more complex the patient, the fewer points you needle. Ask your patient, as you hold the guide tube against the point you are considering, to tell you if it feels like a “yes”. If they scrunch up their face and say “go ahead” through clenched teeth, don’t needle it. You may use fewer needles, finer gauge needles, and not use points they find painful, or too vulnerable.
A needle that comes with a “yes” will carry a healing vibration that one that comes with resistance never could.